How Long Can a Manic Episode Last? A Complete Guide
December 25, 2025 | By Leo Vance
If you or someone you care about is in the midst of a manic episode, you’re likely asking one question: when will this end? Understanding the timeline is a critical step toward managing the situation. So, how long can a manic episode last? While the answer varies, this guide offers a clear overview of the duration, symptoms, and influencing factors. As you read, it can be helpful to complete a bipolar screening questionnaire to organize your thoughts. We’ll explore what to expect with and without treatment, empowering you with the knowledge to find a path toward stability.

What Is a Manic Episode, Exactly?
More than just a good mood, a manic episode is a distinct period of abnormally and persistently elevated or irritable mood, paired with increased energy and activity. This change is a significant departure from a person's usual self and stands as a core feature of Bipolar I Disorder. It is not a fleeting mood swing but a sustained state that impacts daily functioning, relationships, and judgment. Grasping this distinction is key to recognizing the signs.
The Core Signs: Elevated Mood, Energy, and Activity
A manic episode is defined by three core changes: a shift in mood, a surge in energy, and an increase in goal-directed activity. The mood isn’t just happiness; it can be extreme elation or significant irritability. This is often accompanied by a decreased need for sleep, where someone might feel rested after only a few hours. Activity levels ramp up, leading to new projects, ambitious plans, or being far more talkative than usual.
Mania vs. Hypomania: Understanding the Key Differences
While both involve elevated mood, mania and hypomania differ in severity. A full manic episode is severe, lasts at least one week, and causes significant trouble at work or in social settings. Hospitalization may be required for safety. In contrast, hypomania, a hallmark of Bipolar II Disorder, is less severe. While the mood shift is noticeable to others, it doesn't cause major life disruption or include psychotic features, and it lasts at least four consecutive days. If you are trying to understand your own patterns, you can explore these symptom differences in a structured way.
The Duration of a Manic Episode: What to Expect
The primary question — how long can a manic episode last — depends heavily on individual factors, especially treatment. The duration can range from a week to several months. While each person's experience is unique, clinical patterns offer a general timeline. Understanding these timeframes is essential for setting realistic expectations and recognizing the critical role of intervention.
The Baseline: At Least One Week for a Diagnosis
To be clinically diagnosed as manic, symptoms must be present for at least one week, for most of the day, nearly every day. If symptoms are severe enough to require hospitalization, the duration can be shorter. This one-week criterion helps distinguish a manic state from more brief mood fluctuations.
Without Treatment: Episodes Can Last for Several Months
If left untreated, a manic episode can be lengthy and disruptive. On average, an untreated episode can last from three to six months, and some continue for even longer. During this time, the symptoms can cause significant challenges with relationships, work, and finances. Early intervention is incredibly important.
With Treatment: Shortening Episodes and Preventing Recurrence
Effective treatment dramatically changes the prognosis. With the right medication and therapeutic support, the duration of an episode can be significantly reduced, often bringing symptoms under control within weeks. Treatment aims not only to end the current episode but also to prevent future ones, promoting long-term stability.
In Bipolar I vs. Bipolar II: The Role of Mania and Hypomania
The required duration differs based on the diagnosis. Bipolar I is defined by at least one manic episode lasting a week or more. Bipolar II disorder, however, is characterized by a pattern of depressive episodes and the less severe hypomanic episodes.
In a Crisis? What to Do Right Now
If you or someone you know is in immediate danger or experiencing thoughts of self-harm, do not wait.
- Call or text 988 in the U.S. and Canada to reach the Suicide & Crisis Lifeline.
- Call 911 or go to the nearest emergency room for immediate medical help.
- Contact a healthcare provider or a mental health professional as soon as possible.
Your safety is the top priority. Reaching out is the most important step you can take.
Key Symptoms: What a Manic Episode Looks and Feels Like
What does a manic episode look like? It's a combination of emotional, behavioral, and cognitive changes that mark a clear departure from a person's baseline. For the person experiencing it, the world can feel full of endless possibility. To others, their behavior may seem erratic or concerning. These signs are the key to identifying the need for support.
Emotional Signs
The emotional tone of a manic episode can be one of two extremes: an intense, euphoric happiness that feels disconnected from life events, or extreme irritability and anger. A person might have a short fuse and get into arguments easily. At times, these emotional states can shift rapidly.
Behavioral Signs
Changes in behavior are often the most noticeable signs. This includes a significantly decreased need for sleep, where someone might stay up for days on a project yet feel rested. Other common behaviors are rapid speech, being unusually outgoing, and engaging in impulsive or high-risk activities like spending sprees or reckless driving.
Cognitive Signs
Internally, the mind can feel like it’s going a mile a minute. Manic episode symptoms frequently include racing thoughts, making conversation hard to follow. A person may also feel grandiose, believing they have special talents. It becomes very difficult to focus, as their attention is easily pulled to irrelevant details.
What Triggers a Manic Episode and Affects Its Length?
While bipolar disorder has a strong biological basis, specific lifestyle factors can provoke manic episodes. Understanding what sets off an episode is a powerful step toward prevention. Managing these triggers is key to long-term wellness and can help reduce the frequency and severity of future episodes.
Major Life Stress and Upheaval
Significant life events — both positive and negative — can serve as triggers. Situations like losing a job, going through a breakup, or even a big promotion can disrupt routines and increase stress. The resulting emotional and physiological impact can upset the delicate balance of brain chemistry.
Disrupted Sleep Patterns
Lack of sleep is one of the most powerful triggers for mania. The relationship is bidirectional: mania causes a decreased need for sleep, but disrupting a sleep schedule (by pulling an all-nighter or dealing with jet lag) can directly provoke a manic episode. A consistent sleep-wake cycle is a critical strategy for stability.
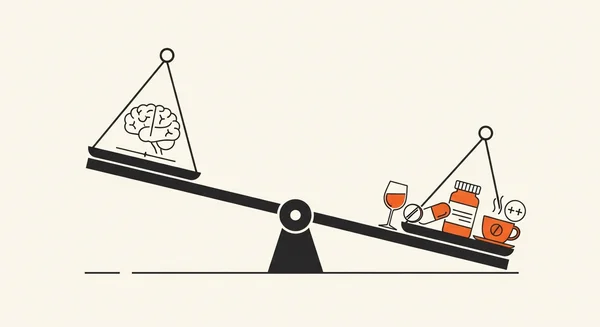
Substance Use and Medications
Certain substances can induce or worsen manic symptoms. Alcohol and recreational drugs are well-known culprits. Additionally, some prescription medications, notably antidepressants taken without a mood stabilizer, can trigger a switch into mania. It's crucial to be open with your doctor about all substances you use.
Strategies to Manage and Shorten Manic Episodes
It is not safe to stop a manic episode on your own. However, professional treatment and proactive strategies can effectively manage it. The goal is to restore balance and prevent recurrence by combining medical treatment, therapy, and lifestyle adjustments. Thinking about how to stop a manic episode immediately should always lead to seeking professional help without delay.
Professional Medical Treatments
Medication is the frontline treatment for managing a manic episode. Mood stabilizers are highly effective at controlling current symptoms and preventing future ones. In some cases, a psychiatrist may use antipsychotic medications for severe signs like agitation. Working closely with a doctor to find the right medication is essential.
The Role of Psychotherapy
Therapy is a vital component of a comprehensive treatment plan. Cognitive Behavioral Therapy (CBT) helps individuals identify and change the thought patterns that accompany mood episodes. Another approach, Interpersonal and Social Rhythm Therapy (IPSRT), is specifically designed to help people stabilize their daily routines, particularly sleep.
Building a Proactive Lifestyle Routine
Beyond professional treatment, a structured lifestyle is a powerful management tool. This includes:
- Consistent Sleep: Go to bed and wake up around the same time daily.
- Stress Management: Incorporate activities like mindfulness, yoga, or hobbies.
- Regular Exercise: Physical activity is a proven mood booster and stress reducer.
- Track Your Moods: Keep a journal to recognize early warning signs.
From Knowledge to Insight: Exploring Your Experiences
Learning about symptoms and triggers is a powerful first step. But how does this general information apply to you specifically? The next step is to organize your thoughts in a structured way, turning abstract concepts into concrete personal reflections. This process isn't about self-diagnosis; it's about gaining clarity.
Structure Your Thoughts for a Clearer Picture
When you're trying to make sense of complex mood changes, your thoughts can feel scattered. A structured approach helps you identify patterns you might have otherwise missed. It provides a clearer, invaluable picture of what you've been going through. This self-exploration empowers you and prepares you to have a more productive conversation with a healthcare professional, should you choose to take that step.
An Educational Tool to Prepare for a Professional Conversation
To help with this process, our confidential Bipolar Disorder Symptom Checker can serve as a guided journal. It's an educational tool designed to help you privately review your experiences against established symptoms. Walking into a doctor's office and saying "I don't feel right" can be daunting. Our tool provides a summary of your responses that you can choose to share with a doctor or therapist, making that conversation much easier and ensuring your provider gets a complete picture from the start.
Ready to gain more clarity? Our tool offers a structured way to review your experiences.
Your Path Forward: Balancing Awareness and Action
Understanding how long a manic episode can last is a critical piece of the puzzle. While an untreated episode can persist for months, effective treatment can shorten its duration. Recognizing symptoms and triggers gives you the power to be proactive.
The path forward involves balancing this awareness with decisive action, such as seeking professional help, building healthy routines, and taking a bipolar disorder test to organize your thoughts. You are not alone.
Frequently Asked Questions
Can a manic episode last for years?
While exceptionally rare, some complex or untreated cases can lead to chronic mood states that last a year or more. However, the standard diagnostic criteria for a single episode outline a much shorter duration.
What does a prolonged manic episode typically look like?
A prolonged episode would likely involve severe disruption to all areas of life, including work and relationships. It could involve psychotic symptoms, significant financial trouble, and would require urgent, intensive professional intervention to stabilize.
Do manic episodes end suddenly or fade out gradually?
It varies. Some people experience an abrupt "crash" where the episode ends suddenly, often transitioning into a depressive state. For others, the symptoms may fade more gradually over days or weeks, with their energy and mood slowly returning to a baseline.
How can you tell the difference between a manic episode in Bipolar I versus Bipolar II?
The key difference is severity. Bipolar I Disorder is defined by at least one full manic episode, which is severe and causes significant life disruption. Bipolar II Disorder involves hypomanic episodes, which are shorter, less severe, and do not include psychosis or require hospitalization.
What is the fastest way to stop a manic episode?
The fastest and safest way to resolve a manic episode is to seek immediate help from a medical professional. There are no "instant" home remedies that can safely stop mania. Professional intervention with medication in a safe environment is crucial for a quick resolution.