Manic Depression — Symptoms, Types, and What It Means Today
February 20, 2026 | By Leo Vance
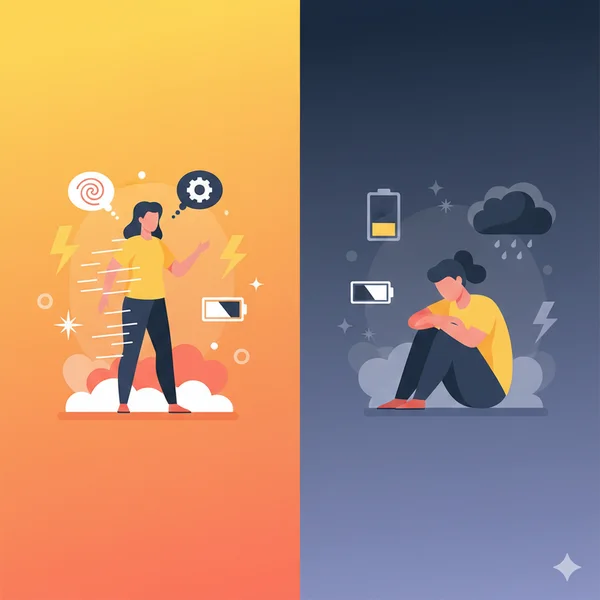
If you've been riding an emotional rollercoaster — weeks of unstoppable energy followed by stretches where getting out of bed feels impossible — you're not alone, and you're not imagining it. Manic depression, now clinically known as bipolar disorder, affects millions of people worldwide. Yet many still search for answers using the older term. This guide walks you through what manic depression really is, the key symptoms and types to understand, how it differs from other conditions, and practical next steps you can take. Whether you're exploring this for yourself or someone you care about, a bipolar disorder test can be a helpful first step toward clarity.

What Is Manic Depression and Why Did the Name Change?
You may have heard both "manic depression" and "bipolar disorder" used to describe the same condition. They do refer to the same illness — but the official name shifted for a good reason.
The term "manic depression" was widely used for decades. However, mental health professionals moved to "bipolar disorder" in 1980 when the DSM-III was published. The newer name does two important things:
- It reduces the stigma attached to the word "manic," which often carries negative connotations.
- It more accurately reflects the two "poles" of mood — emotional highs (mania or hypomania) and lows (depression) — rather than focusing only on the dramatic extremes.
Today, you'll find both terms used interchangeably in everyday conversation. In clinical settings, "bipolar disorder" is the standard. Understanding this context helps you navigate health information more confidently, whether you're reading research or talking to a provider.
How Manic Depression Connects to Bipolar Disorder Types
Manic depression isn't a single experience. It shows up differently depending on the type of bipolar disorder involved:
- Bipolar I — At least one full manic episode, often with depressive episodes too. Mania can sometimes include psychosis.
- Bipolar II — At least one hypomanic episode (less intense than full mania) and at least one major depressive episode. No full-blown mania.
- Cyclothymia — Ongoing mood fluctuations that don't reach the intensity of full manic or depressive episodes, lasting at least two years.
Each type has its own patterns, and recognizing which pattern fits best can guide more effective conversations with a mental health professional.
What Are the Key Symptoms of Manic Depression?
Manic depression symptoms fall into two main categories: those linked to manic (or hypomanic) episodes and those linked to depressive episodes. Many people also experience "mixed episodes," where both types of symptoms overlap.
Signs During a Manic or Hypomanic Episode
- Unusually elevated mood, feeling "on top of the world"
- Dramatically increased energy and reduced need for sleep
- Racing thoughts, rapid speech, and jumping between ideas
- Inflated confidence or grandiosity
- Impulsive decisions — excessive spending, risky behavior, or sudden major life changes
- In severe cases (mania), possible psychosis such as delusions or hallucinations
Signs During a Depressive Episode
- Persistent sadness, emptiness, or hopelessness
- Loss of interest in activities you once enjoyed
- Fatigue and low energy, even after rest
- Changes in appetite or sleep — too much or too little
- Difficulty concentrating or making decisions
- Withdrawal from friends and family
- In severe cases, thoughts of self-harm or suicide
If you or someone you know is experiencing thoughts of suicide, please reach out to the 988 Suicide and Crisis Lifeline (call or text 988) or contact a local emergency service immediately.
What Does a Manic Depressive Episode Actually Look Like?
Daily life during an episode can look very different from the outside. During mania, a person might start three new projects at 2 a.m., max out a credit card, or feel absolutely certain they've had a breakthrough idea — only to crash into deep depression days or weeks later.
During a depressive phase, even small tasks like answering a text or showering can feel overwhelming. The contrast between these states is what makes manic depression so disorienting — for the person experiencing it and for those around them.
How Is Manic Depression Different from BPD and Regular Depression?
One of the most common points of confusion is the difference between manic depression (bipolar disorder), borderline personality disorder (BPD), and major depressive disorder. While they can share overlapping symptoms, they are distinct conditions.
Manic Depression vs. BPD — Key Differences
| Feature | Manic Depression (Bipolar) | Borderline Personality Disorder (BPD) |
|---|---|---|
| Mood shifts | Episode-based (days to weeks) | Rapid, often triggered by interpersonal events (hours) |
| Core driver | Neurobiological mood cycling | Emotional dysregulation and fear of abandonment |
| Self-image | Stable between episodes | Chronically unstable sense of identity |
| Treatment focus | Mood stabilizers, therapy | Dialectical behavior therapy (DBT) |
Manic Depression vs. Major Depression
The main distinction: major depression involves depressive episodes only — there are no manic or hypomanic highs. In manic depression, the presence of at least one manic or hypomanic episode is what sets it apart. This is why someone initially diagnosed with depression might later receive a bipolar disorder diagnosis once a manic or hypomanic episode occurs.
What Triggers Manic Depression and What Are the Risk Factors?
The exact cause of manic depression is not fully understood, but research points to a combination of factors working together.
Biological and Genetic Factors
- Genetics play a strong role. Studies suggest that 80–90% of people with bipolar disorder have a close relative with bipolar disorder or depression.
- Brain chemistry matters. Imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine may contribute to mood instability.
- Brain structure differences have been observed in some imaging studies, though this area is still being explored.
Environmental and Lifestyle Triggers
Even with a genetic predisposition, episodes are often set off by:
- Major life stress — relationship breakdowns, job loss, grief
- Disrupted sleep patterns or chronic sleep deprivation
- Substance use — alcohol and recreational drugs can trigger or intensify episodes
- Traumatic experiences, especially in childhood
Understanding your personal triggers can become a powerful self-management tool over time.
Manic Depression and Psychosis — When Episodes Become Severe
Not everyone with manic depression experiences psychosis, but it can happen — particularly during intense manic episodes. Psychotic features may include:
- Delusions — firmly held false beliefs, such as thinking you have special powers or a unique mission
- Hallucinations — seeing or hearing things that aren't there
Psychosis in the context of manic depression is treatable and temporary. It does not mean someone has a separate psychotic disorder. However, it is a sign that immediate professional support is needed.
If you notice these signs in yourself or someone close to you, reaching out to a mental health professional right away is the most important step.

What Steps Can You Take After Recognizing These Patterns?
Recognizing that your mood patterns might align with manic depression is a meaningful first step. Here's a practical checklist for what to do next:
Your Next-Steps Checklist
- Start tracking your moods. Use a journal or app to record daily energy levels, sleep, and emotional highs and lows. Even two weeks of data can reveal patterns.
- Learn the difference between normal mood changes and clinical episodes. Occasional ups and downs are part of life. Manic depression involves episodes that significantly disrupt daily functioning.
- Try a self-reflection screener. A structured self-screening tool — like our bipolar disorder screening tool — can help you organize your observations before a professional visit. These tools don't diagnose, but they can help you articulate what you've been experiencing.
- Prepare for a professional conversation. Bring your mood tracking notes and screening results to an appointment. Concrete examples help providers understand your experience more quickly.
- Reach out to a mental health professional. A psychiatrist or psychologist can conduct a thorough evaluation, discuss your history, and recommend a treatment path.
Self-screening tools are designed for self-reflection and education. They do not replace a professional diagnosis or clinical evaluation.
When to Seek Help Immediately
Contact a professional or crisis service right away if you experience:
- Thoughts of self-harm or suicide
- Severe sleep deprivation lasting several days
- Behavior that puts you or others at risk
- Psychotic symptoms such as delusions or hallucinations
Wrapping Up — Understanding Manic Depression Is the First Step
Manic depression — or bipolar disorder, as it's known today — is a complex condition, but it is also well-researched and highly treatable. By understanding the symptoms, types, and differences from similar conditions, you're already building a stronger foundation for managing your mental health.
Whether you're here for yourself or for someone you love, the most important thing is to keep moving forward. Track what you notice, ask questions, and don't hesitate to seek professional guidance. If you'd like to organize your thoughts before that conversation, explore the bipolar disorder self-screener to gain a clearer picture of where you stand.
You deserve to understand your own mind — and you don't have to figure it all out alone.
Frequently Asked Questions
What is manic depression called now?
Manic depression is now officially called bipolar disorder. The name was changed in 1980 to better reflect the condition's two mood poles — mania and depression — and to reduce stigma around the term "manic."
Is manic depression the same as bipolar disorder?
Yes, manic depression and bipolar disorder refer to the same condition. "Bipolar disorder" is the current medical term, while "manic depression" is the older, more informal name still widely recognized.
What are the main types of manic depression?
The three primary types are Bipolar I (full manic episodes), Bipolar II (hypomanic and depressive episodes), and Cyclothymia (milder, ongoing mood fluctuations). Each type has different patterns and treatment approaches.
Can manic depression be cured?
There is currently no cure for manic depression, but it can be effectively managed with medication, therapy, and lifestyle adjustments. Many people with bipolar disorder lead full, productive lives with proper treatment.
What is the difference between manic depression and BPD?
Manic depression involves episode-based mood cycling (lasting days to weeks), driven by neurobiological factors. BPD involves rapid emotional shifts often triggered by interpersonal events, with a core pattern of identity instability and fear of abandonment.
How can I tell if my mood swings might be manic depression?
Consider whether your highs involve dramatically increased energy, reduced sleep need, and impulsive behavior — and whether your lows involve persistent sadness and withdrawal. A structured self-screening tool can help you organize these observations for a professional conversation.